In recent years, science has reinforced the central role of intestinal microbiota in maintaining physical and mental health. In addition to actively participating in digestion and immunity, intestinal bacteria also communicate with the brain through a complex system known as gut-brain axis.
This connection has a direct impact on cognitive performance, influencing memory, focus, mood, and even prevention of neurological disorders. For nutritionists and supplement prescribers, understanding this relationship is essential to develop strategies that go beyond conventional nutrition.
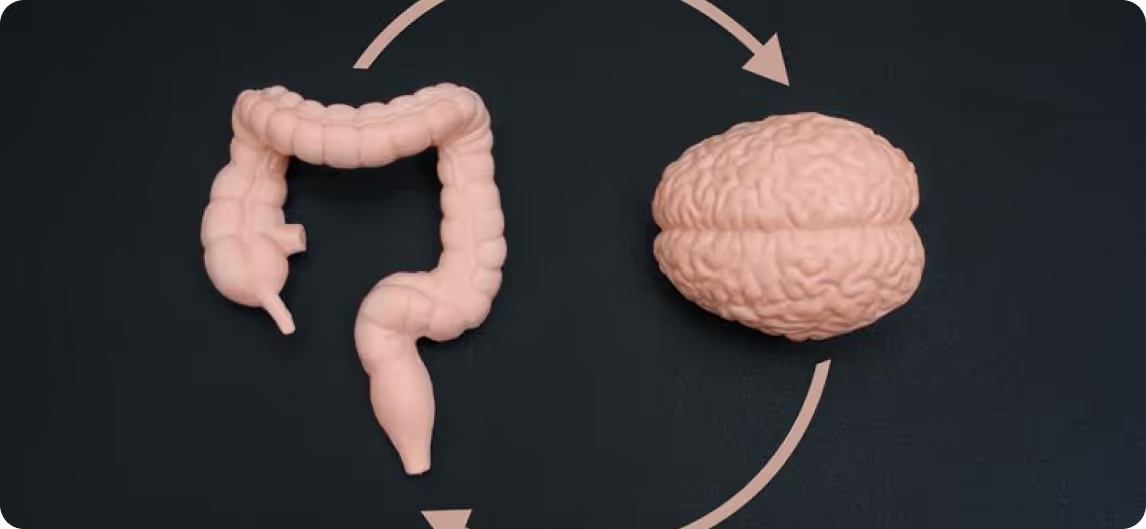
What is the gut-brain axis?
O gut-brain axis is a bidirectional communication system between the gastrointestinal tract and the central nervous system. It involves neural pathways (such as the vagus nerve), immune and metabolic mechanisms, in addition to the influence of metabolites produced by the microbiota, such as:
- Short chain fatty acids (such as butyrate);
- GABA (gamma-aminobutyric acid);
- Serotonin (more than 90% is produced in the intestine);
- Tryptophan and its metabolites.
When this axis is balanced, there is greater emotional stability, mental focus, and lower risk of chronic systemic inflammation.
How does gut microbiota affect cognition?
Several studies have already associated microbiota imbalance (dysbiosis) with cognitive changes. Possible mechanisms include:
- Neurogenic inflammation caused by bacterial endotoxins (such as LPS);
- Reduction Of the synthesis of neurotransmitters, such as serotonin and dopamine;
- Increased oxidative stress in the central nervous system;
- Worsening of neuroplasticity and mitochondrial function.
Patients with complaints such as low concentration, mental fatigue, anxiety, or impaired memory they may be experiencing a silent intestinal dysregulation.
5 signs that the gut microbiota may be affecting cognition
- Recurrent mental fatigue;
- Mood swings without apparent cause;
- Feeling of a “cloudy mind” or forgetfulness;
- Intestinal changes associated with stress or anxiety;
- Sleep is not restorative even with good hours of rest.
The role of the nutritionist and the prescription of supplements
The nutritionist is a key player in modulating intestinal microbiota in a personalized way. Based on clinical signs and dietary history, it is possible to implement behaviors that promote intestinal health and, as a consequence, mental health.
Among the most effective strategies are:
- Specific probiotics, like Lactobacillus rhamnosus GG and Bifidobacterium longum, already studied for their anxiolytic and cognitive effects;
- Prebiotics (such as FOS, GOS, and inulin), which feed good bacteria;
- Glutamine, which regenerates the intestinal mucosa and reduces local inflammation;
- Polyphenols and antioxidants, such as turmeric and resveratrol, which protect the nervous system and microbiota;
- Tryptophan, Magnesium, and B Vitamins, important for the production of neurotransmitters.
Vitafor's line of supplements offers complete support for these interventions, with highly bioavailable active ingredients and scientific support.
Healthy microbiota
Keep a balanced intestinal microbiota it's not just a therapeutic measure, it's a strategy of primary prevention. In times of mental overload, overuse of antibiotics, inflammatory diets, and sleep disorders, the gut becomes even more vulnerable.
By acting on the intestine, nutritionists promote more than digestion: they promote emotional stability, focus, and sustainable cognitive performance.
Conclusion
A intestinal microbiota is a powerful ally in promoting brain health. For health professionals who wish to act more fully, understand the gut-brain axis and using supplementation as a clinical tool is an increasingly valued differential.
Taking care of the intestine is, yes, taking care of the brain. And this integrated, science-based approach is what modern patients expect from their reference professionals.